||| BY THOMAS O. BALDWIN, PhD |||
As a result of amazing strides in basic biomedical science over the past several decades—development of methods allowing the cloning of genes, DNA sequencing, etc.— it has been possible to develop several exceptionally effective vaccines against COVID-19 over the past year, an accomplishment that usually takes several years to a decade. These vaccines were developed without cutting any corners in testing of safety and efficacy, an accomplishment that clearly demonstrates what can be accomplished when government and private labs work together toward a common goal. Yet, today, for reasons that I do not understand, there are people in the United States who are reluctant to get the vaccine. Whether it is due to disinformation about the vaccines that has been spread by Russia and/or China and/or Iran, or some other source of conspiracy theories, the result is the same—many people are reluctant to get vaccinated. That is unfortunate for several reasons. First, a vaccine is a fast, safe method to acquire immunity to the disease without suffering with the disease and potentially dying from it. Furthermore, if too many people refuse the vaccine, we cannot reach “herd immunity,” a situation that will be harmful to all of us, and prolong the time until we can return to a more normal life style.
SO, WHAT IS “HERD IMMUNITY”?
When one person within a population is infected by the SARS-CoV-2 coronavirus and suffers with and then recovers from COVID-19, that person will generally be immune to a second infection. The same is true for individuals who are vaccinated—they are not susceptible to an infection by the novel coronavirus, unless, through mutations that might occur when the virus replicates, mutants emerge that can escape the defense mechanisms that your body establishes following an infection or vaccination against the original form of the virus. For the virus to spread within a population, there must be susceptible individuals in the population. If people are not susceptible, as a result of either having the disease or vaccination, the disease cannot spread. If people are not susceptible, it’s almost as if they are not there, as the virus cannot replicate in their bodies. The larger the proportion of immune individuals in the population, the more difficult it is for the virus to spread. This is the condition known as “herd immunity”. The proportion of the population that must be immune to slow and then stop the spread of the disease depends on how easily spread the virus is within a sensitive population. If the virus spreads very easily, as is the case with measles, herd immunity requires that almost the entire population be immune. If the virus spreads less easily, herd immunity will be achieved at a lower proportion of immune individuals. If there were no variant strains of the COVID-19 virus that are more transmissible, it has been estimated that herd immunity would be achieved when 70-80% of the population world-wide has either had the disease or has been vaccinated.
To better understand herd immunity, consider the graphic below–
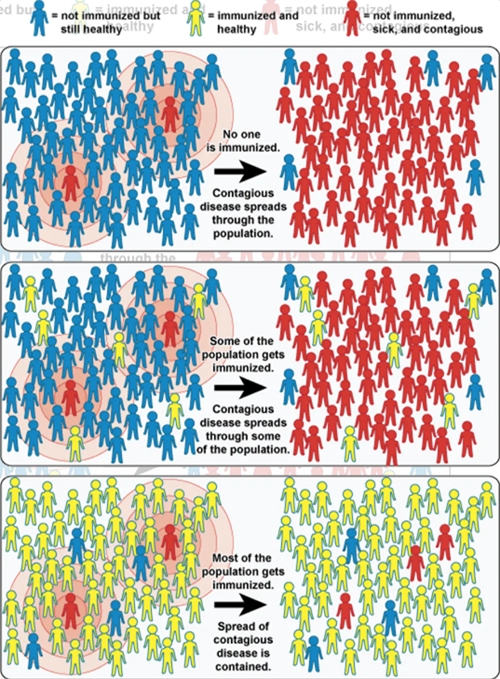
Graphic from the National Institute of Allergy and Infectious Disease
This graphic depicts three situations. In the top panel, none of the population have been vaccinated. When people carrying the contagious disease come into the population, the disease spreads to most of the population. In the middle panel, some in the population have been vaccinated, but not very many. When the disease enters the population, it spreads to the unvaccinated individuals just as if none of the population were vaccinated. In the bottom panel, most of the individuals have been vaccinated. Now, when the disease enters the population, there are so few sensitive individuals that the disease cannot get a foothold and spread. This is called herd immunity.
SUGGESTIONS THAT mRNA VACCINES WILL MODIFY OUR DNA ARE UNFOUNDED
Depending on the source and the method of calculation, the number of cells in the human body is thought to be between 1 trillion and 100 trillion. All of those cells came from a single cell—the result of the fusion of an egg and a sperm cell. Each of those trillions of cells has the same DNA content in its nucleus, half of which came from the egg and half from the sperm. Yet, there are many types of cells in our bodies—skin, many types of blood cells, muscle, bone, etc.—even though the DNA content of each is the same. It is widely appreciated that the DNA of the cell contains the instructions, the blueprints, that determine our many bodily characteristics. So, if the instructions are the same in every cell, why are there so many different types of cells that are so very different?
The DNA in your cells is organized into genes, each gene carrying the instructions for a specific function. These genes are the heritable units that collectively determine such characteristics as your skin, hair and eye color, your height, the shape of your ears and nose, and all other characteristics. Individual genes have control circuits that turn them on and off depending on conditions. Different genes are expressed in different types of cells, resulting in the different characteristics of the different cell types, even though the DNA content is the same. After an egg is fertilized by a sperm cell, the resulting cell divides multiple times to create a cell mass. After several divisions, cells begin to “differentiate,” turning certain genes on and others off, such that certain groups of cells become nervous tissue, others become skin, others become bone, and so forth, with each cell type having only a subset of all genes being functional.
Science fiction stories that suggest reprogramming an adult human’s DNA have one primary problem—it’s the many trillions of cells that comprise the adult human. Modifying the DNA of
a single cell isn’t simple, but it is possible. But how to make the same change in each of those trillions of cells? That’s why it’s called science fiction.
Today, there are individuals who claim that the new mRNA-based vaccines that provide protection against SARS-CoV2 infection (COVID-19) are a plot perpetrated by Bill Gates, Microsoft, the Democrats, or any number of other potential villains. Those claims, too, fall into the category of science fiction. I will try to explain why that is true by explaining how vaccines work, and in closing, with a focus on the mRNA vaccines.
A BRIEF HISTORY OF VACCINES AND VACCINATIONS
Vaccination began in 1796 during a smallpox outbreak in England. It had been known for centuries that if someone caught smallpox, or any number of other infectious diseases, and survived, they would most likely not get the disease a second time. Edward Jenner, a country physician, had long noticed that people who spent a lot of time milking cows did not get smallpox. Cows have a similar disease known as cowpox that causes the same sort of blisters as smallpox in humans, but does not make the cows so sick. Jenner wondered if it were possible that people could become infected with cowpox, showing minimal if any symptoms, and thereby become immune to infection by smallpox. This could explain the so-called “milkmaid’s complexion,” as milkmaids could be immune to smallpox by virtue of prior infection by cowpox.
To test his hypothesis, Jenner took a small amount of pus from a cowpox blister and injected it under the skin of an 8-year-old boy who had never had smallpox. The boy developed a slight fever and lost his appetite, but in a few days, regained full health. That summer, when the smallpox outbreak was raging across England, Jenner took a small amount of pus from a blister of one of his patients and injected it under the skin of the boy. As Jenner had expected, the boy developed no symptoms. He was the first person successfully vaccinated against smallpox. As we now know, the cowpox virus is sufficiently similar to the smallpox virus that immunity to cowpox affords immunity to smallpox.
Four years later, Jenner’s method of vaccination against smallpox was widely used across England, much of Europe, and the United States. Jenner died in 1823. By that time, the incidence of smallpox had been slashed in half, and by 1979, smallpox had been eradicated worldwide, so that smallpox vaccinations are no longer necessary for the general public. Since the time of Edward Jenner, much has been learned about infectious diseases and the human immune system. While helping the silk industry in France to fight a disease in silkworms in the 1870s, Louis Pasteur discovered that the disease was caused by a fungus. This discovery led Pasteur to propose the germ theory of infectious diseases. Shortly thereafter, while working on a cholera epidemic in chickens, Pasteur discovered that injection of weakened cultures of the causative bacteria into healthy chickens prevented them from developing the disease. In the 1880s, Pasteur proposed using other techniques, such as heating, drying, etc., to weaken strains of bacteria for use in vaccinations. His work led him to develop a successful vaccination against rabies utilizing weakened rabies virus. For many years, this was the method employed to vaccinate against infectious diseases, and in short order, we had vaccines against tuberculosis, typhoid fever and cholera.
Over the following decades, using much the same approach, scientists developed vaccines against polio, mumps, measles, rubella, and chickenpox. We learned not only how to create a vaccine that would elicit immunity to a specific infectious agent, we learned how the body responds to vaccinations to develop that immunity, just as if we had had the disease, but without actually having the disease.
HOW DOES YOUR BODY’S IMMUNE SYSTEM RESPOND TO AN INFECTION, OR A VACCINE?
This story has many players, but the central theme relies on protein molecules called antibodies. Antibodies are proteins that can recognize foreign proteins or other substances on the surfaces of invading bacteria, fungi or viruses. With the help of an array of cells in our bodies, the antibodies target the invaders for destruction. Antibodies can distinguish between molecules that are normal components of our bodies, and molecules that reside on the surface of an invading bacterium, virus or fungus. Antibodies can recognize and bind to these foreign proteins. When an antibody binds to some foreign molecule, the cells that produce that specific antibody are stimulated to replicate to produce more of that antibody. The part of the foreign molecule to which the antibody binds is called an antigen. The invading agent will likely have many antigens on its surface and thus will elicit amplified production of an array of antibody molecules, each binding to a specific antigen. Binding of antibodies to the surface of an infectious agent marks it as a foreign species and other cells in the body then will attack and destroy the infectious agent.
Understanding this, scientists found that vaccines do not have to be made from whole cells of an infectious agent. Instead, they can take one of the proteins on the surface of an infectious agent, and use that protein as a vaccine, with none of the dangerous parts of the disease agent involved. Understanding such details of the immune system led scientists to propose that vaccines did not need to be made from weakened or dead whole cells of the infectious agent. Rather, purified components of the infectious agent could be used, especially if the component was from the external surface of the invading agent.
RECOMBINANT VACCINES
Today, scientists can find a harmless protein on the surface of an infectious agent and use it in a vaccine. Since only the surface protein is in the vaccine, not the infectious “disease-causing” agent, there is no possibility of the vaccination causing the disease. Development of recombinant DNA technology has allowed cloning of the genes from infectious agents that encode specific surface components. Cloning allows production of large amounts of a single protein from large cultures of the recombinant organism. The purified protein can then be used in a vaccine against the original virulent agent. In such “recombinant” vaccines, no weakened or inactivated disease-causing agent is injected, so there is no way the vaccine can cause the disease. The possibility of inadvertently causing the disease via vaccination, even in a few individuals, is eliminated. Today, there are many variations on this general theme of vaccine development, depending upon the characteristics of the specific disease and its causative agent. The principle is the same—antibodies to a protein of the infectious agent bind to it, marking that protein and therefore the invading virus, bacterium or fungus for destruction by your immune system.
mRNA VACCINES—BACKGROUND CONCEPTS
With the emergence of the SARS-CoV2, or the novel coronavirus, and its attendant COVID-19 disease, a new path to immunization that was already in development for other purposes has been deployed with great success. This approach utilizes mRNA, or messenger ribonucleic acid, as the active agent in the vaccine rather than a component of the virus itself. To understand how this method works requires a little understanding of nucleic acids (DNA and RNA).
DNA, or deoxyribonucleic acid, is a huge molecule that is a string of units abbreviated as G, A, T, and C. DNA resides in the nucleus, and it is the stuff that comprises all the genes that make us who we are. DNA is a very stable molecule—so much so that it is possible to extract DNA from teeth of animals that died long ago, and to sequence that DNA to learn about genes from organisms long extinct. RNA, on the other hand, is exceptionally unstable, usually breaking down in a matter of a few minutes to a few hours. A specific kind of RNA, mRNA, is a copy of a gene within the DNA in the nucleus that is made in the nucleus and then moves out of the nucleus into the cellular juice called cytoplasm. In the cytoplasm, there are molecular machines called ribosomes that bind to mRNA, read the sequence of the units, which is determined by the sequence of units (G, A, T and C) in the original nuclear DNA, and translate the sequence of the mRNA into a sequence of amino acids that results in the formation of a specific protein.
This biological function of mRNA requires that it be comparatively unstable. When the gene is turned on, mRNA is produced, which then moves into the cytoplasm where it is translated into protein. That protein has some specific function, and when there is enough of it, the cell signals the gene to stop making the mRNA. So that the protein is not produced after the gene is turned off, it is essential that the mRNA break down quickly. The mRNA has a short life-time in the cell—the amount of a specific mRNA present at any time is determined by its rate of synthesis in the nucleus and its rate of breakdown in the cytoplasm.
HOW DO mRNA VACCINES WORK TO PROTECT AGAINST COVID-19?
With this background, we can now explore how mRNA vaccines work. In the case of the coronavirus that causes COVID-19, the target selected for immunization is called the spike protein. There are many copies of the spike protein decorating the surface of the coronavirus. These spike proteins can be seen in the microscopic images of the virus, which appears as a sphere with spikes all over its surface. This spike protein is the “handle” that attaches to specific cells in our respiratory systems to allow the virus to enter our cells. The mRNA for the vaccine carries the code to instruct cells to make the spike protein; the vaccine does not contain the spike protein itself. The mRNA in the vaccine enters the cell’s cytoplasm, and once in the cytoplasm, the ribosomes will bind the mRNA, read the instructions, and produce the spike protein. The nature of the spike protein is to insert into membranes, just as it does with the virus, and the new spike proteins will therefore move into your cell’s membrane and protrude through to the outside. From there, your immune system will see these spike proteins as foreign molecules and mount an immune response. A graphic representation of how the vaccines work is presented below.
But if mRNA is so unstable, how can a vaccine be made using the mRNA for the spike protein to instruct our cells to produce the spike protein, a “foreign” protein against which our immune system will make antibodies? Scientists working on this technology learned that they could “package” the mRNA into tiny lipid “bubbles,” and inside these bubbles (called vesicles), the mRNA would be much more stable. But the mRNA is still intrinsically unstable, which is why these vaccines must be kept cold. When the vaccine is injected into your muscle, the lipid vesicles fuse with the membranes surrounding your cells, delivering the mRNA to the cytoplasm. Then, just as with mRNA coming out of the nucleus in the normal functioning of your cells, your ribosomes read the spike protein mRNA sequence and translate it into an amino acid sequence that defines the spike protein of the coronavirus. Once your cells produce the spike protein, your immune system will mount an immune response. But since the mRNA is so unstable, it breaks down fairly quickly, so there is a limited amount of the spike protein made, resulting in a relatively low immune response from the first injection. Three or four weeks later, when you get a booster (second dose) of the mRNA vaccine, your immune system is primed, so when the spike protein is made the second time, your immune response will be much stronger.
But why use the mRNA for the spike protein as a vaccine rather than the spike protein itself? Cloning the gene for the spike protein, expressing the recombinant protein in large tanks, and purifying the protein is a difficult and time-consuming process. Synthesizing a relatively short strand of RNA is very simple and fast, and if you want to try several sequences, it is fast and simple to do so. It is clear that mRNA vaccines have much to recommend them, and I am sure they will be with us for many years to come.
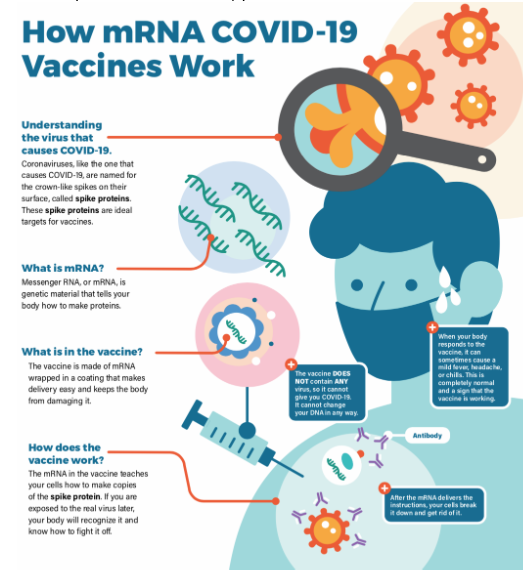
Graphic taken from the Center for Disease Control and Prevention website
Recent studies have shown that the mRNA vaccines can dramatically enhance the immunity caused by a natural infection with the virus. Researchers studied two groups—those who had not tested positive for the coronavirus, and those who had tested positive but had not been hospitalized. The researchers monitored the level of the antiviral antibody produced in each group following first one, and then a second (3-4 weeks later) injection of either the Pfizer or Moderna mRNA vaccine. For the control group, those who had never tested positive for the virus, the response was what we normally see—first, a modest level of antibody production followed by a robust response to the second injection. For the group of individuals who had tested positive for the virus but had not had a case of the disease requiring hospitalization, the first injection resulted in a very strong response, a far greater immune response than that after even the second injection for the control group. The response to the second injection for the experimental group was stronger still, but the difference from the first injection was not as great as for the control group. These studies demonstrate the potential value of providing vaccinations even to those who have tested positive, and this is especially true if variants of the virus emerge that are able to evade to some extent the defense afforded by the initial exposure to the virus.
These new mRNA vaccines show promise in medical science beyond the immediate application to fighting the coronavirus pandemic. One promising area is in the field of immunotherapies for cancer treatment. Cancer vaccines are a form of immunotherapy, where the vaccine instructs the immune system to attack the cancer. Personalized cancer vaccines, where the mRNA sequence in the vaccine is designed to code for specific protein(s) on the cancer cells, are being explored. Over 50 clinical trials are currently underway for mRNA vaccines in a number of cancers, including blood cancers, melanoma, brain cancer and prostate cancer. Immunotherapy is distinct from chemotherapy, surgery and radiation, and while it will not replace these older treatments anytime soon, recent progress is very exciting.
Bottom line—the vaccines against COVID-19 work, the vaccines approved by the FDA for use in the U.S. are safe, and for the good of all, anyone who is not immunocompromised or has any other medical condition that precludes vaccination, should be vaccinated. Herd immunity is good for us all, and the sooner we get there, the sooner we can all return to something like pre-COVID normalcy.
Note that the Federation of American Societies for Experimental Biology (FASEB) has published a very informative document entitled Vaccines: Essential Weapons in the Fight Against Disease. The report was published several years ago, before the mRNA vaccines had been developed. That document can be found HERE.
Tom Baldwin received his BS and PhD from the University of Texas at Austin. He did postdoctoral training at Harvard University, and began his career in the Biochemistry Department of the University of Illinois, Urbana. In 1981, he moved his laboratory to Texas A&M University where he worked for 18 years. He was recruited to the University of Arizona as Professor and Head of the Department of Biochemistry and Molecular Biophysics. In 2008, he was recruited to the University of California, Riverside, as Professor of Biochemistry and Dean of the College of Natural and Agricultural Sciences. He retired in 2015, and now lives full time on Orcas Island with his wife, Dr. Miriam Ziegler, who is also a biochemist.









This was a fabulous article, clearly explaining how the Covid19 vaccines work (super cool) , why they are safe, and why we should take them. Every Science class should read this.
Kudos to Dr. Baldwin for providing one of the most lucid and succinct public letters I have seen on the state of the art and science of vaccines. I did not know that the very concept of vaccines and vaccinations had been around, and generally accepted, for 225 years. Thank you Tom!
Yes, an excellent summary article that goes into good detail about the new mRNA vaccines made by Pfizer and Moderna (the one that most of us on Orcas Island have received or will receive). Worth adding is the fact that these two vaccines appear to be effective against the most common coronavirus variant, the B.1.1.7 variant that ravaged Britain in late 2020 and has been growing rapidly in the US in early 2021, according to recent research. The jury is still out on other variants like the South African B.1.351 and Brazilian P.1, but it’s likely that the mRNA vaccines will offer some level of protection against these, too. Whether that will be enough is still an open question.